QUERCC
Quantifying, Understanding and Enhancing Relational Continuity
of Care
Background of the study
Relational continuity of care (RCC) is the extent to which patients see the same clinicians over time. It is linked to better health outcomes and patient experience, and is valued by clinicians. However, RCC is declining, partly due to increasing practice size, part-time working, staff and patient turnover. Most general practices neither measure nor monitor their own RCC and may be unaware how within-practice policies affect it. In choosing a measure, practices need to consider how it fits their own objectives. The effect of practice-level characteristics – practice size, part-time working, staff and patient turnover – on RCC is unquantified. As a result, we do not know how much changes in these characteristics will affect RCC, or if they can be mitigated by within-practice policies.
We know some practices have higher RCC than expected, given their characteristics. Learning from them could provide valuable knowledge on optimising RCC. Although health and resource benefits of RCC are well recognised, no economic analysis has evaluated the overall effects on health outcomes and resource use (prescribing, consultations, hospital admissions) or whether the economic case for RCC differs between population groups (e.g. older vs. younger patients). Most importantly, to optimise RCC, practices need realistic guidance, which is adaptable to their own context.
QUERCC study main aim is to understand how to optimise relational continuity of care in primary care
Objectives
1. Develop guidance for general practices on measuring RCC
2. Quantify the effects of staff and patient turnover, part-time working and practice size on RCC
3. Understand how some general practices achieve high RCC
4. Develop practical guidance to help general practices optimise RCC
5. Undertake economic analysis of the effects of changing RCC
Methods

First, in two consensus workshops of patients, primary care clinicians and researchers, we will develop an understanding of RCC and guidance to help practices select measures.
Second, in a large primary care database, we will model the association between practice RCC and practice-level characteristics (practice size, staff and patient turnover, part-time working). Having determined predictors of RCC we will identify practices showing higher-than-expected RCC (positive deviants) for investigation as case studies.
Third, in depth case studies of positive deviant practices will explore staff and patient experience, trade-offs between access and continuity, and identify practice policies contributing to RCC.
Fourth, we will undertake economic analysis of the projected effects of RCC, using linked primary and secondary care data. We will stratify the analysis by age, sex, deprivation and chronic disease status.

Fifth, in two workshops of clinicians, researchers and patients, we will co-design empirically-informed practical guidance to improve RCC. This will synthesise findings of our quantitative analyses, case studies, and existing continuity of care research in the UK and internationally. Patient and public involvement (PPI) is embedded in the project, through quarterly consultation with a patient advisory group chaired by our PPI co-applicant. Lay participants will be trained in and contribute to analysis of qualitative data.
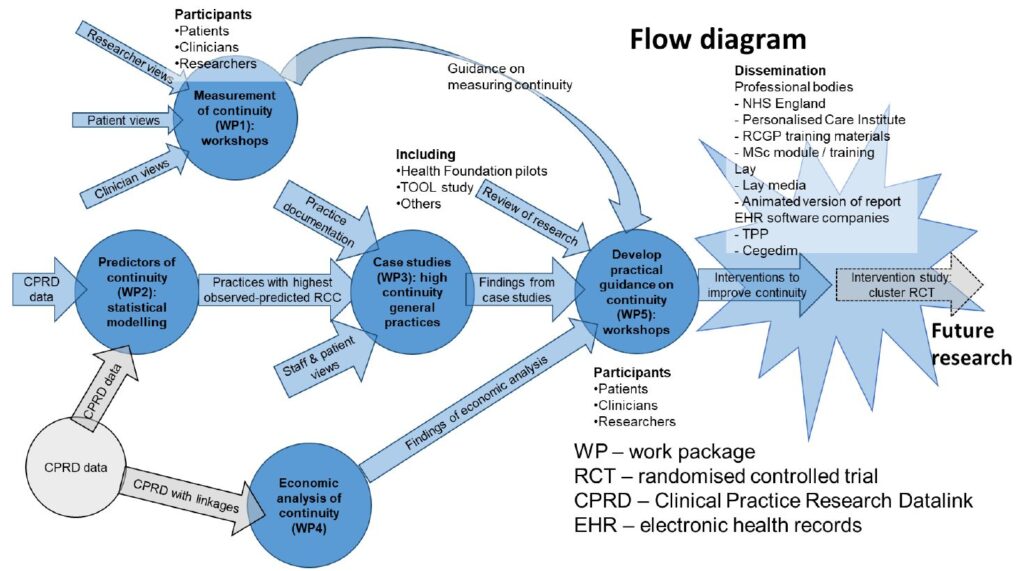
Timeline: 36 months
Impact and dissemination: Alongside academic dissemination, we will report to NHS England, develop training materials for the Royal College General Practitioners and for our own MSc programme. Following this we will evaluate an intervention to improve RCC as a cluster RCT.