QUERCC
Quantifying, Understanding and Enhancing Relational Continuity
of Care
Project Update no. 7: August 2024
Continuity of care (CoC) refers to the consistent and seamless provision of healthcare services to a patient over time, which clinicians and patients highly value for its numerous benefits. However, there has been a consistent decline in CoC within NHS English general practices. The provision of CoC is indeed complex, and one of the challenges is identifying all influencing factors.
In Work Package 2 (WP2), we are examining various elements affecting CoC, such as workload, staff turnover, multiple morbidity, and the age distribution of the patient population, among other factors. It is fascinating to study how they correlate with various measures of the CoC indices. One of the most interesting aspects of our research is identifying the subtle ways in which these elements interact to influence continuity, including the direction and magnitude of their effects across different CoC indices.
As researchers, we are enjoying the challenge of piecing together these insights. Using the largest primary care datasets, CPRD Aurum and GOLD, we are getting closer to understanding the bigger picture. It is like solving a complex puzzle where every piece is crucial. Moreover, although the general trend in CoC is declining, some practices continue to offer reasonable CoC. In WP2, we also aim to identify these general practices that maintain higher levels of continuity of care, learn from their approaches, and conduct focus group interviews (WP3). This will help us develop actionable strategies that can be shared across general practices to help reverse the decline in CoC and ultimately improve patient outcomes and satisfaction.
Project Update no. 6: July 2024
Work package 3 has necessary approvals in place and site selection is in progress. We are currently working with regional CRN to set up at case study sites and focus groups with patients and staff will commence after the summer recess.
The paper presented by Dr Jinyang Chen (Research Fellow, Centre for Health Economics, University of York) at the Health Economists’ Study Group (HESG) summer conference 2024 was well received and the team are working on feedback obtained.
The team are planning a second training session for PPI members, the first explored the basics of Health Economics, following on from this and in response to PPI interest the team will provide an overview of how qualitative researcher use principles of Normalisation Process Theory in the new academic term. Professor Iestyn Williams will be leading a review of the literature on RCC in the coming months and the team are working on a draft paper and report of the findings from WP1. Professor Tom Marshall the study PI is working on ideas for a follow up study and has placed a call for a PhD student to join the team on the PhD Programmes, Research Projects & Studentships in the UK & Europe (findaphd.com).
Project Update no. 5: July 2024
Project Update no. 4: May 2024
On the morning of 9th May 2024, the QUERCC team hosted an online workshop on workload, staffing, productivity and continuity of care. This impromptu online workshop brought together researchers and analysts with interests in workload, staffing, productivity and continuity of care in primary care. There will be short presentations and a wide discussion about the factors affecting demand for primary care consultations, how continuity of care influences demand, the effects of staffing turnover on continuity of care clinical outcomes, how staffing and funding affect patient experience.
The idea was the brainchild of a conversation between Tom Marshall and Steve Wyatt (of The Strategy Unit). Steve had recently published three reports. One on long-term trends in GP practice consultation rates, a second on the gap between need for and supply of GP practice consultations and a third on GP practice productivity, efficiency, and continuity of care. He pointed out that some current policies intended to increase access (using allied health professionals to provide care, policies to divert patients to community pharmacies, creating hubs to provide acute primary care) may also reduce continuity. Two analyses have shown that lower continuity may increase demand for consultations: one by Harshita Kajaria-Montag and the other a PhD thesis by Anas El Turabi. Other researchers have investigated staffing and patient experience and the link between good clinical care and staff turnover in general practice. So we decided to invite these researchers to take part in an online meeting and see if we could generate more research ideas. All the invited researchers were very enthused and interested in the issues raised, so the workshop was born.
‘We’re hoping to get a better understanding of how current policies are impacting continuity of care and how this might be affecting general practice. It will be good to get a lot of expertise thinking about this at the same time, to see what ideas are generated.’
Project Update no. 3: March 2024
Project Update no. 2: February 2024
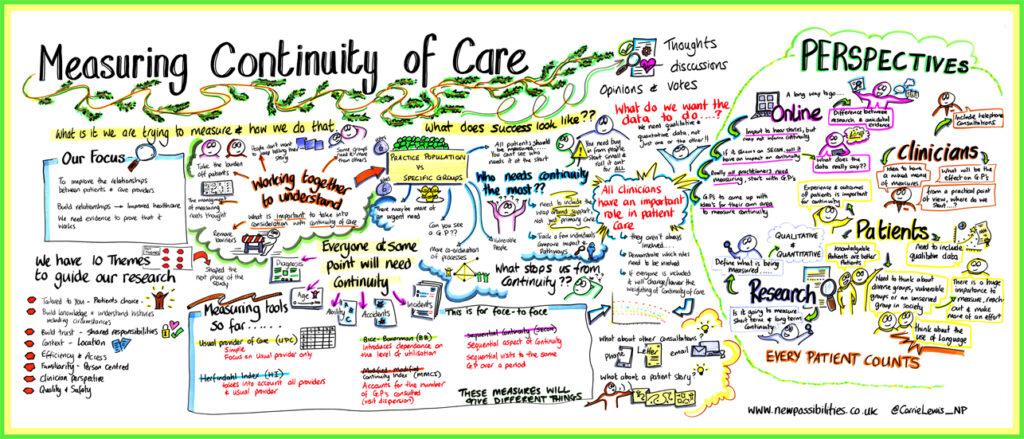
We invited a sample of the same participants back to join us for a second workshop to debate the question of ‘How to measure continuity of care and for which patient groups?’ For general practices to know how well they are delivering continuity of care, they need to measure it. There are several different ways of measuring continuity which are calculated from the pattern of consultations. Our work on QUERCC aims to clarify these issues for general practice and the workshops provide important sensitising information for us to take forward to the next stages of the research. Working with team from New Possibilities our researchers illustrated the range of ways that continuity can be measured to participants, and participants voted on scenario’s we described. The slides illustrating a range of measurement scenarios are available here. New Possibilities produced a visual summary of the discussion which highlighted the complexity of the issues in hand.
Project Update no.1: November 2023
The QUERCC team held the first in a series of two workshops exploring the meaning and measurement of continuity of care in general practice on Friday 24 November at the Exchange central Birmingham. Thirty members of the public [representing patients, health care professionals and researchers involved in primary care research] joined the workshop to debate ‘what continuity of care means to you’. The workshop used coproduction methods to ensure all participants and especially patients had their view listened to. It was led by facilitators from the Birmingham based New Possibilities and their team produced a visual summary of the narrative of the discussion and core themes. Findings from this workshop correspond broadly with previous research which highlights the way in which continuity is valued because it delivers patient choice, trust and person-centred care.
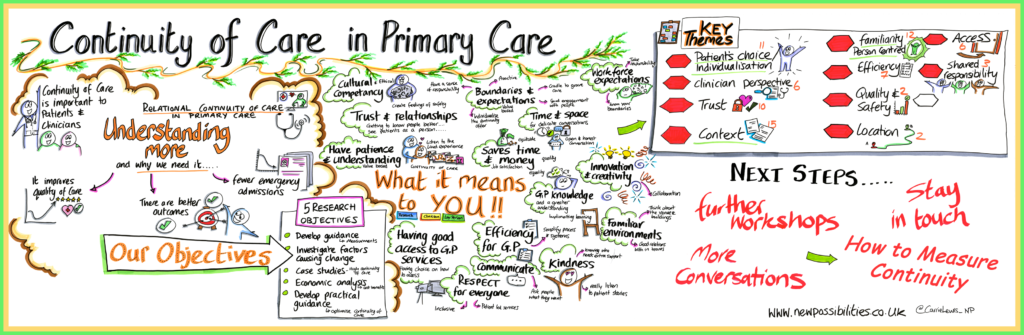
The data collected in this workshop will contribute to the development of a shared understanding of continuity of care to guide the choice of measurement indices.